

Starting dialysis is rarely considered “too late,” as research shows that delaying treatment does not significantly increase mortality risks. Studies reveal that patients initiating dialysis later, even with severe symptoms, experience similar survival rates compared to those starting earlier. This finding highlights the importance of individual health assessments when determining the right time to begin treatment. Dialysis plays a crucial role in managing advanced kidney disease, offering symptom relief and improving daily functioning for many patients. However, decisions about when to start dialysis should always involve careful discussions with healthcare providers to align with the patient’s medical needs and personal goals.
Key Takeaways
- It is almost never too late to start dialysis.
- Doctors decide timing based on each person’s health needs.
- Waiting too long can make symptoms worse and cause problems.
- Serious issues like heart failure can happen if dialysis is delayed.
- Planning early with doctors can prevent emergencies and help recovery.
- Patients’ choices and health should guide when to begin dialysis.
- Other care options might work better for older or very sick patients.
Understanding Dialysis
What Dialysis Does?
Replacing Kidney Function to Remove Waste and Toxins
Dialysis serves as a life-saving treatment for individuals with advanced kidney disease. When kidneys lose their ability to filter waste, toxins, and excess fluids from the blood, dialysis steps in to perform this critical function. By removing harmful substances, dialysis helps maintain the body’s chemical balance and prevents complications like uremia, which can lead to severe health issues.
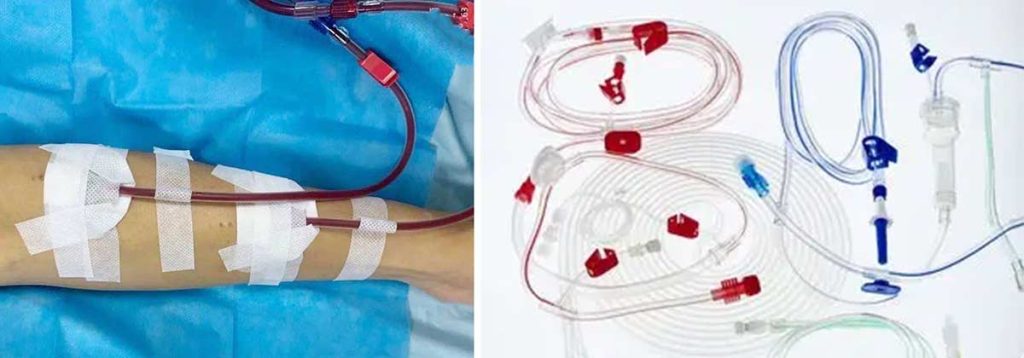
Types of Dialysis: Hemodialysis and Peritoneal Dialysis
There are two primary types of dialysis: hemodialysis (HD) and peritoneal dialysis (PD). Hemodialysis involves using a machine to filter blood outside the body, typically performed three to four times a week at a clinic or hospital. In contrast, peritoneal dialysis uses the lining of the abdomen (peritoneum) as a natural filter. This method can be done daily at home, offering greater flexibility and convenience for patients. Studies suggest that at-home dialysis, when supported by proper education, can improve clinical outcomes and enhance quality of life.
| Study Focus | Key Findings |
|---|---|
| DIALOGICA Study | Highlights the need for high-quality studies comparing dialysis and conservative care. |
Why Patients Start Dialysis?
Managing End-Stage Kidney Disease (ESKD)
Patients with end-stage kidney disease often start dialysis to manage symptoms and maintain their health. Clinical guidelines recommend initiating dialysis when the estimated glomerular filtration rate (eGFR) falls between 5 and 10 ml/min/1.73 m². This decision is typically based on the presence of uremic symptoms, such as nausea, fatigue, or swelling, which indicate the kidneys can no longer function adequately.
Preventing Complications from Kidney Failure
Starting dialysis at the right time can prevent severe complications associated with kidney failure. Delaying treatment increases the risk of volume overload, which can lead to heart failure and other life-threatening conditions. Research shows that dialysis patients who start dialysis based on laboratory evidence of kidney function decline have better survival rates compared to those who delay treatment due to symptoms alone.
| Evidence Type | Description |
|---|---|
| Clinical Guidelines | Dialysis initiation typically occurs when eGFR is between 5-10 ml/min/1.73 m². |
| Mortality Risk | Starting dialysis due to volume overload increases mortality risk by 1.69 times. |
Factors That Influence When to Start Dialysis
Medical Indicators
Kidney Function Tests (e.g., GFR Levels)
Kidney function tests, particularly the glomerular filtration rate (GFR), play a critical role in determining when to start dialysis. GFR measures how well the kidneys filter waste from the blood. A lower GFR indicates declining kidney function. Clinical guidelines suggest initiating dialysis when GFR levels fall below specific thresholds. For example:
| GFR Level (mL/min/1.73m²) | Recommendation |
|---|---|
| ≤ 6 | Dialysis initiation recommended as a sole criterion (Canadian Society of Nephrology). |
| < 8 | Conservative treatment advised until this level, even with symptoms (Japanese Society for Dialysis Therapy). |
| < 2 | Dialysis initiation strongly recommended (Japanese Society for Dialysis Therapy). |
| 15-16 | Associated with lower mortality risk compared to levels of 6-7 (Fu et al. study). |
These thresholds provide a framework, but individual symptoms and overall health often guide the final decision.
Symptoms Like Fatigue, Swelling, and Nausea

Symptoms of kidney failure, such as persistent fatigue, swelling in the legs or feet, and nausea, often signal the need to start dialysis. These symptoms result from the buildup of toxins and excess fluid in the body. Addressing these issues early can prevent complications like uremia or heart failure. Dialysis patients experiencing these signs should consult their healthcare provider to evaluate whether dialysis is necessary.
Overall Health
Impact of Comorbidities on Dialysis Timing
Comorbidities, such as diabetes, heart disease, or chronic obstructive pulmonary disease (COPD), significantly influence the timing of dialysis. Studies show that patients with higher comorbidity scores often face increased risks during dialysis. For instance:
| Study | Findings | Comorbidities Impact | eGFR Impact |
|---|---|---|---|
| Liu et al. | No significant survival differences among groups with varying eGFRs. | Adjusted for age, gender, diabetes, etc. | No significant impact on survival. |
| Chang et al. | Late and very late initiation had similar mortality hazards. | Indicators of comorbidity (e.g., 3-5 and 6-7). | No advantage on long-term prognosis. |
| Zhang et al. | Comorbidities like cerebrovascular diseases and COPD linked to mortality. | Charlson comorbidity index significantly associated. | eGFR at initiation not significant. |
Patients with severe comorbidities may require earlier intervention to manage complications effectively.
Balancing Risks and Benefits for Elderly Patients
Elderly patients often face unique challenges when starting dialysis. While dialysis can improve symptoms, it may also lead to increased hospitalizations and longer recovery times. Healthcare providers must weigh the potential benefits against the risks, considering the patient’s overall health and life expectancy. For some elderly individuals, conservative management may offer a better quality of life.
Quality of Life
Weighing the Benefits of Dialysis Against Its Impact on Daily Life
Dialysis can alleviate symptoms and improve physical health, but it also demands significant time and lifestyle adjustments. Patients undergoing dialysis often report fewer symptoms like pain or discomfort compared to those opting for conservative care. However, hospitalization rates are higher among dialysis patients, with longer median admission days (7 days) compared to conservative care patients (4 days). These factors highlight the importance of evaluating how dialysis will affect daily routines and long-term well-being.
Patient Goals and Preferences in Treatment Planning
Patient-centered care is essential when deciding to start dialysis. Some individuals prioritize extending life, while others focus on maintaining independence and minimizing medical interventions. Healthcare providers should discuss treatment options, including conservative care, to align with the patient’s values and goals. For patients over 80, studies show no significant differences in 12-month survival rates between those starting dialysis and those choosing conservative care, emphasizing the importance of personal choice.
Risks of Delaying Dialysis
Worsening Symptoms
Increased Fatigue, Swelling, and Fluid Retention
Delaying dialysis can lead to a noticeable decline in physical well-being. Dialysis patients often experience worsening fatigue, swelling in the limbs, and fluid retention. These symptoms occur because the kidneys can no longer remove excess fluids and toxins effectively. Over time, this buildup can make daily activities more challenging and reduce overall quality of life.
Missed dialysis sessions, often caused by emergencies like power outages or lack of clean water, have been linked to serious health issues. These include electrolyte imbalances and increased visits to emergency departments. Dialysis patients who live alone or have been on dialysis for fewer than two years are particularly vulnerable to these risks.
Risk of Severe Complications Like Uremia or Heart Failure
Prolonged delays in starting dialysis increase the likelihood of severe complications. Uremia, a condition caused by the accumulation of waste products in the blood, can lead to confusion, nausea, and even seizures. Additionally, fluid overload may strain the heart, raising the risk of heart failure. Clinical data highlights the correlation between delayed dialysis and escalating complications:
| Indication for Dialysis Initiation | Risk of Subsequent Mortality |
|---|---|
| Laboratory evidence of kidney function decline (reference category) | Lowest |
| Uremic symptoms | Moderate |
| Volume overload or hypertension | Highest |
| Other/unknown | N/A |
Organ Damage
Effects of Untreated Kidney Failure on Other Organs
Untreated kidney failure does not only affect the kidneys. It can also harm other vital organs. For example, the heart and lungs may suffer due to fluid buildup, while the liver and gastrointestinal system may struggle with toxin overload. These effects can lead to a cascade of health problems, making recovery more difficult.
Long-Term Consequences of Delaying Treatment
The longer dialysis is delayed, the greater the risk of irreversible damage. Chronic exposure to high toxin levels can impair cognitive function and weaken the immune system. This makes patients more susceptible to infections and other complications. Early intervention helps mitigate these risks and preserves overall health.
Emergency Dialysis
Risks of Starting Dialysis in a Crisis Situation
Starting dialysis during a medical emergency often results in poorer outcomes. Dialysis patients may require intensive care, which increases the risk of complications. Emergency dialysis also limits the opportunity for proper planning, such as choosing the most suitable type of dialysis or preparing the body for treatment.
Importance of Proactive Planning to Avoid Emergencies
Proactive planning ensures a smoother transition to dialysis. Regular monitoring of kidney function and symptoms allows healthcare providers to recommend the best time to start dialysis. This approach reduces the likelihood of emergencies and improves long-term outcomes.
When Dialysis May Not Be Recommended?
Advanced Age
Risks and Benefits for Elderly Patients
For elderly patients, the decision to start dialysis requires careful consideration of risks and benefits. Research shows that initiating dialysis in older adults with multiple health conditions often does not extend life expectancy compared to conservative management. The GOLD Study monitored patients aged 65 and older for six months after starting dialysis or opting for conservative care. Results revealed no significant improvement in quality of life for dialysis patients, while those choosing conservative care experienced a clinically relevant decline. Hospitalization rates were also higher among dialysis patients, with 50% requiring hospital care compared to 24% in the conservative care group.
| Statistic | Value |
|---|---|
| Percentage of new dialysis patients aged 70+ (2019) | 45% |
| One-year mortality rate for patients aged 70+ | 18% |
| Five-year mortality rate for patients aged 70+ | 72% |
Alternative Approaches to Managing Symptoms
For elderly individuals, alternative approaches such as conservative management may provide better outcomes. This approach focuses on symptom control, maintaining comfort, and improving quality of life without dialysis. Healthcare providers often recommend this option for patients who prioritize minimizing medical interventions over extending life expectancy.
Severe Comorbidities
When Other Health Conditions Make Dialysis Less Effective?
Severe comorbidities can reduce the effectiveness of dialysis. Conditions like advanced cardiovascular disease, diabetes, or chronic obstructive pulmonary disease (COPD) often complicate treatment. The Cumulative Illness Rating Scale-Geriatrics (CIRS-G) assesses comorbidity burden, with a score of ≥2x score 3 or ≥1x score 4 indicating severe conditions. Patients with high comorbidity scores may experience limited benefits from dialysis and face increased risks during treatment.
- Studies highlight the importance of individualizing treatment plans for patients with severe comorbidities.
- Worsening cardiovascular symptoms and advanced age often influence the choice of dialysis modality.
Palliative Care as an Alternative to Dialysis
Palliative care offers a viable alternative for patients with severe comorbidities. This approach prioritizes symptom relief and emotional support, helping patients maintain dignity and comfort. It also allows individuals to focus on their personal goals without the physical and emotional demands of dialysis.
Patient Choice
Respecting a Patient’s Decision to Decline Dialysis
Patients have the right to decline dialysis if it does not align with their values or goals. For many, the decision reflects a desire to avoid the burdens of treatment and focus on quality of life. Studies like the DIALOGICA project emphasize the importance of understanding individual preferences when discussing renal replacement therapy.
Supporting Patients with Non-Dialysis Care Options
Healthcare providers play a crucial role in supporting patients who choose non-dialysis care. Presenting dialysis as a palliative treatment can help frail older adults understand their options. Framing treatment as symptom-alleviating rather than life-prolonging allows patients to weigh the trade-offs and make informed decisions. This approach ensures that care aligns with the patient’s priorities and enhances their overall well-being.
Conclusion
Starting dialysis is rarely considered too late, but the decision should align with individual health, symptoms, and personal goals. Delaying treatment can lead to complications like worsening symptoms or emergency dialysis. Proactive planning with healthcare providers helps avoid these risks. A comprehensive review of studies highlights the complexity of dialysis timing, emphasizing the need to balance clinical symptoms, GFR levels, and quality of life. In some cases, alternative care approaches may better suit patient preferences. Consulting with a healthcare team ensures informed decisions tailored to each situation.
