

Medicaid plays a vital role in providing dialysis treatment for individuals diagnosed with end-stage renal disease (ESRD). Nearly half of all Americans undergoing dialysis depend on Medicaid to fund their care. This program ensures access to essential services, including treatment in dialysis center and home dialysis options. However, the specifics of Medicaid cover dialysis services vary by state. Eligibility requirements and additional costs depend on individual circumstances, making it important for dialysis patients to understand their state’s Medicaid program.
Key Takeaways
- Medicaid pays for important dialysis care, like in-center treatments and home dialysis lessons. This helps patients get care without money problems.
- Medicaid rules are different in each state. Patients should check their state’s rules to know what is covered and any limits.
- People with both Medicaid and Medicare save more money. Medicaid helps pay for things Medicare doesn’t fully cover.
- Dialysis patients should call their state Medicaid office to check their benefits. They can also read their Medicaid plan to learn what is covered.
- Looking into extra help programs or charities can cover costs Medicaid doesn’t pay for. This makes it easier to get the care they need.
Medicaid Cover Dialysis Services
What Services Are Included?
In-Center Dialysis Treatments
Medicaid provides coverage for dialysis treatments in center, which are essential for individuals with end-stage renal disease (ESRD). These treatments involve regular visits to dialysis centers, where patients receive care from trained professionals. Medicaid ensures that eligible individuals can access these life-saving services without financial barriers. According to healthcare data, nearly half of Americans undergoing dialysis rely on Medicaid for funding, highlighting its critical role in supporting ESRD patients.
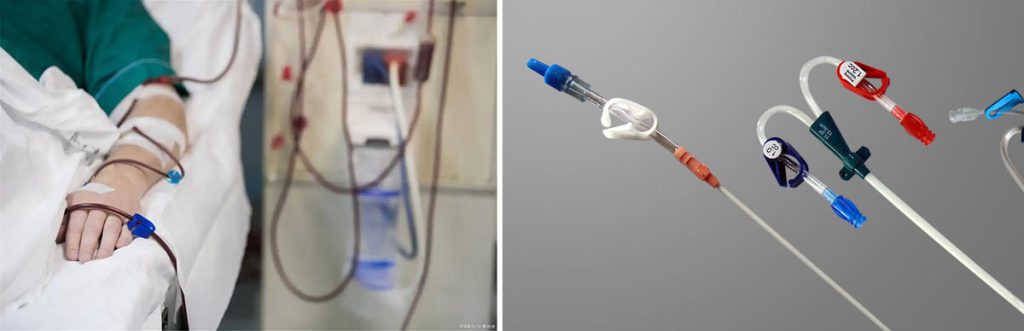
Home Dialysis Training and Equipment
For dialysis patients who prefer or require home-based care, Medicaid covers home dialysis training and equipment. This includes the necessary machines, supplies, and training for patients and caregivers to perform dialysis safely at home. Home dialysis offers flexibility and convenience, allowing patients to manage their treatment schedules more effectively. Medicaid’s support for home dialysis reflects its commitment to providing comprehensive care options tailored to individual needs.
Medications and Supplies for Dialysis
Medicaid also covers medications and supplies essential for dialysis treatment. These include drugs to manage complications associated with ESRD, such as anemia or bone disease, and supplies like dialyzers and tubing. By covering these costs, Medicaid helps reduce the financial burden on patients and ensures they receive the full spectrum of care required for effective treatment.
Are There Coverage Limitations?
State-Specific Variations
Medicaid coverage for dialysis services can vary significantly by state. Each state administers its Medicaid program, which means the extent of coverage and specific services included may differ. Dialysis patients should review their state’s Medicaid guidelines to understand what is covered and any potential limitations.
Prior Authorization Requirements
Some states may require prior authorization for certain dialysis-related services. This means patients or providers must obtain approval from Medicaid before receiving specific treatments or supplies. Understanding these requirements is crucial to avoid delays in care. Medicaid enrollees should work closely with their healthcare providers to navigate these processes effectively.
Eligibility for Medicaid Dialysis Coverage
General Medicaid Eligibility
Income and Asset Requirements
Medicaid eligibility depends on income and asset limits, which vary by state and applicant category. For most children, pregnant women, and adults, the Modified Adjusted Gross Income (MAGI) methodology simplifies the process by assessing taxable income without considering assets. However, individuals aged 65 or older or those with disabilities often qualify through non-MAGI pathways, which include specific asset limits. These limits differ by state and eligibility group, ensuring that Medicaid supports those with the greatest financial need.
The Affordable Care Act introduced the MAGI methodology to streamline Medicaid applications. This approach excludes asset tests for most applicants, making it easier for families and individuals to qualify. Non-MAGI pathways, however, still require applicants to meet both income and asset criteria, reflecting the program’s focus on assisting vulnerable populations.
Residency and Citizenship Criteria
Medicaid applicants must meet residency and citizenship requirements to qualify for coverage. Individuals must reside in the state where they apply and demonstrate legal citizenship or eligible immigration status. States may request documentation, such as proof of residency or citizenship, during the application process. These criteria ensure that Medicaid resources are allocated to eligible residents who need assistance.
Dialysis-Specific Eligibility
ESRD Diagnosis and Medical Necessity
Medicaid cover dialysis for individuals diagnosed with end-stage renal disease (ESRD), a condition requiring life-saving treatment. ESRD often results from chronic kidney disease caused by diabetes or hypertension. By 2018, over 750,000 Americans were living with ESRD, highlighting the growing need for dialysis services. Medicaid ensures that patients with a confirmed ESRD diagnosis receive the necessary treatment to manage their condition.
To qualify for dialysis coverage, dialysis patients must demonstrate medical necessity. This involves a physician’s confirmation that dialysis is essential for the patient’s survival. Medicaid’s focus on medical necessity ensures that resources are directed toward individuals with critical health needs.
Documentation Requirements
Applicants seeking Medicaid coverage for dialysis must provide specific documentation. This includes medical records confirming an ESRD diagnosis and evidence of medical necessity. States may also require additional paperwork, such as proof of income, assets, and residency. Accurate and complete documentation helps streamline the approval process, ensuring timely access to dialysis treatment.
Medicaid and Medicare for Dialysis Patients
Dual Eligibility for Medicaid and Medicare
How Dual Eligibility Works?
Patients with dual eligibility can access both Medicaid and Medicare benefits, which work together to provide comprehensive dialysis care. Medicare typically serves as the primary payer, covering the majority of dialysis-related expenses. Medicaid acts as a secondary payer, addressing costs that Medicare does not fully cover, such as copayments, deductibles, and additional services. This coordination ensures that patients receive the necessary treatment without excessive financial strain.
Note: Medicaid can also provide coverage during the initial waiting period before Medicare benefits begin, ensuring uninterrupted access to dialysis services.
Benefits of Dual Coverage
Dual eligibility offers several advantages for dialysis patients. It reduces out-of-pocket expenses by covering costs that Medicare alone might not handle. Medicaid also provides additional support, such as transportation to treatment centers and coverage for medications not included under Medicare. This dual-layered approach enhances access to essential care and minimizes financial challenges for patients managing end-stage renal disease.
Coverage Coordination and Timelines
Medicare’s Waiting Period for Dialysis
Medicare coverage for dialysis typically begins at the start of the fourth month after the first treatment session. During the initial three months, dialysis patients may face a gap in funding. However, Medicaid can step in to cover dialysis costs during this waiting period, ensuring patients receive uninterrupted care. In some cases, Medicare may waive the waiting period if the patient completes a Medicare-approved home dialysis training program.
Medicaid as a Secondary Payer
Medicaid plays a crucial role in covering costs that Medicare does not fully address. For example, it can pay for services like transportation to dialysis centers or additional treatments not covered by Medicare. Medicaid also supports patients during the 30-month coordination period when Medicare serves as the primary payer. This collaboration ensures that patients receive comprehensive care without financial barriers.
| Coverage Type | Description |
|---|---|
| Medicare | Coverage for dialysis starts at the fourth month after the first treatment session. |
| Medicaid | Can be used during the qualifying period before Medicare coverage begins. |
Patients with dual eligibility benefit from seamless coordination between Medicaid and Medicare, ensuring access to life-saving dialysis treatments.
Costs and Patient Responsibilities
Medicaid Coverage for Dialysis Costs
Treatment and Transportation Costs
Medicaid provides essential support for individuals undergoing dialysis. It covers most of the costs associated with dialysis treatments, ensuring that patients with end-stage renal disease (ESRD) can access life-saving care. Nearly half of all Americans receiving dialysis rely on Medicaid to help pay for their treatment. This program also addresses transportation needs, which are critical for patients who must travel to dialysis centers multiple times a week. Medicaid ensures that eligible individuals can reach their treatment locations without financial strain.
Additional Covered Services
Medicaid coverage extends beyond dialysis treatments and transportation. It includes other necessary services, such as medications to manage complications from chronic kidney disease and supplies required for dialysis procedures. For patients who choose home dialysis, Medicaid also covers training and equipment. These comprehensive benefits reduce the financial burden on patients and ensure they receive the care needed to manage their condition effectively.
Out-of-Pocket Expenses
Coinsurance and Deductibles
While Medicaid covers a significant portion of dialysis costs, dialysis patients may still face some out-of-pocket expenses. For individuals with dual eligibility for Medicaid and Medicare, Medicare Part B typically covers 80% of dialysis costs. Medicaid often steps in to cover the remaining 20%, including coinsurance and deductibles. This coordination minimizes financial challenges for patients, ensuring they can focus on their treatment.
Costs Not Covered by Medicaid
Despite its extensive coverage, Medicaid may not cover all expenses related to dialysis. For example, certain over-the-counter medications or non-essential supplies might fall outside the scope of Medicaid coverage. Patients should review their Medicaid plan carefully to understand any potential gaps. Exploring alternative support options, such as nonprofit organizations or financial assistance programs, can help address these additional costs.
Confirming Medicaid Coverage for Dialysis
How to Verify Your Medicaid Benefits?
Contacting Your State Medicaid Office
Verifying Medicaid benefits begins with contacting the state Medicaid office. Each state administers its Medicaid program, so the specific details of dialysis coverage may vary. State Medicaid representatives can provide accurate information about eligibility, covered services, and any required documentation. Patients should prepare their Medicaid ID and relevant medical records before reaching out. This ensures a smoother process when discussing dialysis-related inquiries.
Reviewing Your Medicaid Plan
Another effective way to confirm dialysis coverage is by reviewing the Medicaid plan. Patients can access their plan details through the Medicaid website or by requesting a printed copy. The plan outlines covered services, including dialysis treatment, medications, and transportation. It also highlights any limitations, such as prior authorization requirements. Understanding the plan helps patients anticipate potential costs and avoid unexpected expenses.
Medicaid plays a crucial role in covering dialysis for individuals with end-stage renal disease (ESRD). This coverage typically addresses most dialysis costs, especially during the initial 90 days before Medicare benefits begin. Patients should take proactive steps to verify their benefits to ensure uninterrupted access to life-saving treatment.
Exploring Alternative Support Options
Financial Assistance Programs

For patients facing financial challenges, various assistance programs can help cover dialysis-related expenses. Some states offer additional Medicaid waivers or grants to support individuals with ESRD. These programs may address costs not fully covered by Medicaid, such as home dialysis equipment or specialized medications. Patients should inquire about these options through their state Medicaid office or local healthcare providers.
Nonprofit Organizations for Dialysis Patients
Nonprofit organizations also provide valuable support for dialysis patients. Groups like the American Kidney Fund and the National Kidney Foundation offer financial aid, educational resources, and emotional support. These organizations often assist with transportation, medication costs, and other essential needs. Patients can explore these resources to supplement their Medicaid benefits and reduce the financial burden of dialysis treatment.
Tip: Patients should combine Medicaid benefits with alternative support options to maximize their access to comprehensive care.
Conclusion
Medicaid plays a critical role in ensuring access to dialysis for individuals with end-stage renal disease. Patients must verify their eligibility and understand their coverage details to avoid unexpected costs. Maintaining a regular dialysis schedule at home is essential for continued eligibility and immediate funding. This understanding helps patients and stakeholders plan effectively for treatment. For those requiring additional assistance, exploring nonprofit organizations or financial aid programs can provide valuable support.
Tip: Patients should regularly review their Medicaid plan and consult their state Medicaid office to stay informed about their benefits.
