
Dialysis plays a crucial role in managing fluid overload in the body by effectively helping to remove fluid from the bloodstream. This process alleviates symptoms caused by overhydration and supports better overall health. Clinical studies have demonstrated significant success in how dialysis removes fluid during treatments. For instance:
- At four weeks, dialysis patients experienced an average reduction of 0.96 liters in overhydration volume.
- By twelve weeks, this reduction increased to 1.06 liters, contributing to improved fluid balance.
While dialysis removes fluid from the bloodstream efficiently, it does not directly address fluid in the lungs. Conditions like pulmonary edema, which lead to lung fluid accumulation, require specialized treatments beyond dialysis.
Key Takeaways
- Dialysis helps remove extra fluid from the blood. This helps control fluid buildup and improves health.
- Dialysis does not directly take fluid from the lungs. But it can help lungs work better by lowering body fluid pressure.
- Ultrafiltration is the main way dialysis removes fluid. Careful control is needed to prevent problems like low blood pressure.
- Problems like fluid in the lungs often need special treatments. These include water pills or oxygen therapy, not just dialysis.
- Watching your health and changing habits, like drinking less and eating better, can help people with lung fluid problems feel better.
How Does Dialysis Remove Fluid?
Understanding Dialysis
What Is Dialysis and How Does It Work?
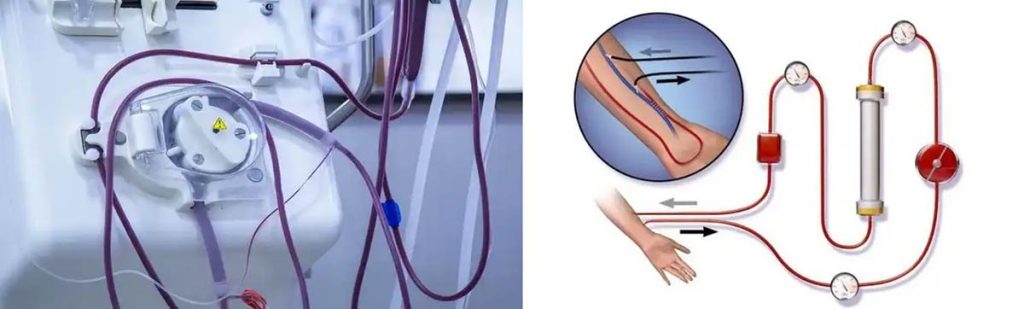
Dialysis is a medical procedure designed to perform the functions of healthy kidneys in individuals with kidney failure. It removes waste products, toxins, and excess fluid from the bloodstream. This process helps maintain a balance of electrolytes and fluids in the body. Dialysis works by using a semi-permeable membrane to filter blood, allowing unwanted substances to pass through while retaining essential components like blood cells and proteins.
Types of Dialysis: Hemodialysis vs. Peritoneal Dialysis
There are two primary types of dialysis: hemodialysis and peritoneal dialysis. Hemodialysis involves circulating the patient’s blood through a machine equipped with a dialyzer, which acts as an artificial kidney. In contrast, peritoneal dialysis uses the lining of the abdomen (the peritoneum) as a natural filter. A special fluid is introduced into the abdominal cavity to absorb waste and excess fluid, which is then drained out. Both methods aim to achieve the same goal but differ in their approach and suitability for patients.
The Role of Dialysis in Fluid Management
How Dialysis Removes Excess Fluid from the Bloodstream?
Dialysis removes excess fluid from the bloodstream through a process called ultrafiltration. This technique creates a pressure difference across the dialysis membrane, drawing water from the blood into the dialysate. The rate of fluid removal is carefully controlled to prevent complications. For example, fluid movement between body compartments occurs at a regulated pace, ensuring that the body can adapt to changes in fluid levels.
- Ultrafiltration is the primary method for fluid removal during dialysis.
- In hemodialysis, fluid is drawn from the blood into the dialysate due to pressure differences.
- The ultrafiltration rate is adjusted based on the patient’s fluid weight gain to achieve the target dry weight safely.
The Importance of Ultrafiltration in Fluid Removal
Ultrafiltration plays a critical role in maintaining fluid balance in dialysis patients. It ensures that excess fluid is removed without causing harm. However, removing fluid too quickly can lead to complications. Research highlights that for every 0.5 milliliter increase in fluid removed per kilogram of body weight per hour, the risk of death rises significantly. This underscores the importance of precise fluid management during dialysis.
Accurate assessment tools like bioimpedance analysis and lung ultrasound are emerging as valuable methods for evaluating fluid status. These tools provide more precise evaluations than traditional methods, reducing the risk of complications such as hypertension and heart failure.
Dialysis and Fluid Overload
How Fluid Overload Affects the Body including the Lungs?
Fluid overload occurs when the body retains more fluid than it can handle. This condition can lead to swelling, high blood pressure, and strain on the heart. In severe cases, it causes fluid to accumulate in the lungs, resulting in pulmonary edema. This condition makes breathing difficult and reduces oxygen levels in the blood.
Dialysis as a Tool to Manage Fluid Overload
Dialysis serves as an effective tool for managing fluid overload. By removing excess fluid from the bloodstream, it helps alleviate symptoms and prevent complications. Studies show that structured interventions, such as nurse-led protocols and patient education, improve hydration status and overall outcomes for dialysis patients. These approaches emphasize the importance of accurate fluid assessment and adherence to treatment plans.
Can Dialysis Remove Fluid from the Lungs?
Why Dialysis Does Not Directly Remove Lung Fluid?
Differences Between Fluid in the Lungs and Fluid in the Bloodstream

Fluid in the lungs, known as pulmonary edema, differs from fluid in the bloodstream. Pulmonary edema occurs when fluid leaks into the air sacs of the lungs, impairing oxygen exchange. In contrast, fluid in the bloodstream circulates throughout the body and can be directly accessed during dialysis. Dialysis remove fluid from the bloodstream by filtering it through a semi-permeable membrane, but it cannot directly target fluid trapped in the lungs.
Medical studies highlight the challenges of addressing lung fluid through dialysis. For example:
- Traditional fluid assessment methods in dialysis patients often fail to detect localized fluid buildup in the lungs.
- Ultrasound-based techniques, while promising, require skilled operators and may not always identify the root cause of pulmonary congestion.
- Rapid fluid removal during dialysis can increase the risk of complications, including pressure on the lungs.
Limitations of Dialysis in Addressing Localized Fluid Buildup
Dialysis has limitations when dealing with localized fluid accumulation in the lungs. Diagnostic tools like lung ultrasounds and chest X-rays provide valuable insights but have constraints.
| Diagnostic Tool | Limitation |
|---|---|
| Lung Ultrasound (LUS) | Limited in identifying the exact cause of pulmonary congestion. |
| Chest X-ray | Detects pulmonary edema only when significant volume overload is present. |
| Operator Dependency | Requires skilled operators; lung pathologies can affect interpretation. |
These limitations emphasize the need for alternative treatments to address lung-specific fluid buildup.
When Dialysis Can Help with Lung Fluid?
Cases Where Reducing Overall Fluid Overload Improves Lung Function
Although dialysis does not directly remove lung fluid, it can indirectly improve lung function by reducing overall fluid overload. Excess fluid in the body increases pressure on the lungs, leading to respiratory issues. By removing fluid from the bloodstream, dialysis alleviates this pressure, improving breathing and oxygen levels. Studies show that nearly two-thirds of critically ill patients with acute kidney injury experience fluid overload, and routine fluid removal during dialysis helps relieve lung pressure.
Examples of Conditions Where Dialysis Is Part of the Treatment Plan
Certain conditions benefit from dialysis as part of a broader treatment plan. For instance:
- Pulmonary edema caused by kidney failure often improves when dialysis removes excess fluid.
- Respiratory complications like pneumonia linked to fluid overload may also see improvement with effective fluid management.
- Research highlights the acute effects of hemodialysis on pulmonary function, showing a clear relationship between fluid status and respiratory health.
In these cases, dialysis plays a supportive role in managing fluid overload, indirectly benefiting lung function.
Limitations and Risks of Dialysis for Lung Fluid
Risks Associated with Dialysis
Side Effects Such as Low Blood Pressure
Dialysis can cause side effects, including low blood pressure, especially during or after fluid removal. Rapid fluid removal places stress on the cardiovascular system, leading to a sudden drop in blood pressure. This condition, known as intradialytic hypotension, can cause dizziness, nausea, and even fainting. Managing fluid removal rates is critical to avoid these complications.
Research highlights the dangers of removing fluid too quickly. A study published in JAMA Network Open found that faster fluid removal increases the risk of death in the months following dialysis. For every 0.5 mL increase in fluid removed per kilogram of body weight per hour, the risk of death rises significantly. Critically ill patients who underwent fluid removal at rates exceeding 1.75 mL/kg/hr faced a 51% to 66% higher risk of death within three months. These findings emphasize the importance of balancing fluid removal to prevent low blood pressure and other complications.
Risks of Over-Removing Fluid During Dialysis
Over-removing fluid during dialysis can lead to severe health issues. Excessive fluid removal may cause dehydration, cramping, and reduced blood flow to vital organs. This can result in long-term damage to the heart and kidneys. Clinicians must carefully monitor patients to ensure that only the necessary amount of fluid is removed.
The challenge lies in accurately assessing fluid levels. Traditional methods, such as physical examinations and blood pressure measurements, often fail to provide precise evaluations. The table below outlines some limitations of these methods:
| Evidence Type | Description |
|---|---|
| Volume Overload | Excess extracellular fluid leading to venous and pulmonary congestion. |
| Traditional Assessment Limitations | Clinical parameters like blood pressure and physical examination often mislead volume status evaluation. |
| Detection Methods | Chest X-ray detects pulmonary edema only at significant overload levels. |
These limitations highlight the need for advanced tools and careful management to avoid over-removing fluid during dialysis.
Situations Where Dialysis May Not Be Effective
Non-Fluid-Related Causes of Pulmonary Edema
Pulmonary edema can result from factors unrelated to fluid overload, such as heart failure, infections, or lung injuries. In these cases, dialysis may not provide relief, as it targets fluid in the bloodstream rather than addressing the underlying cause. For example, heart failure-induced pulmonary edema requires treatments like medications to improve heart function rather than dialysis.
Cases Requiring Alternative Treatments
Certain conditions demand alternative treatments beyond dialysis. For instance, pulmonary edema caused by infections or trauma may require antibiotics or surgical interventions. Oxygen therapy and mechanical ventilation often play a crucial role in stabilizing patients with severe lung fluid buildup. Dialysis serves as a supportive measure in some cases but cannot replace targeted treatments for non-fluid-related causes.
Note: Dialysis is a valuable tool for managing fluid overload, but its effectiveness depends on the underlying cause of lung fluid accumulation. Consulting a healthcare provider ensures the most appropriate treatment plan.
Alternative Treatments for Fluid in the Lungs
Medications for Pulmonary Edema
Diuretics and Their Role in Removing Lung Fluid
Diuretics play a key role in managing pulmonary edema by helping the body eliminate excess fluid. These medications, particularly loop diuretics like furosemide, reduce fluid buildup in the lungs and improve breathing. They work by increasing urine production, which lowers fluid levels in the bloodstream and decreases pressure in the lungs. Clinical data supports their effectiveness, especially in patients with acute respiratory distress syndrome (ARDS) or severe lung injury.
| Evidence Summary | Findings |
|---|---|
| Loop diuretics and ARDS | Reduced 28-day mortality in ARDS patients, especially with high CVP. |
| Fluid management strategies | Conservative fluid management improved oxygenation and reduced mortality. |
| EVLW reduction | Decrease in extravascular lung water (EVLW) correlated with better survival. |
Other Medications to Address Underlying Causes
In addition to diuretics, other medications target the root causes of pulmonary edema. For example, vasodilators like nitroglycerin reduce the workload on the heart in cardiogenic pulmonary edema. Antibiotics treat infections that may lead to lung fluid buildup. Beta-blockers and ACE inhibitors improve heart function, preventing further fluid accumulation. These treatments complement dialysis in cases where kidney failure contributes to fluid overload.
Medical Interventions
Oxygen Therapy and Mechanical Ventilation
Oxygen therapy provides immediate relief for patients struggling to breathe due to lung fluid. It increases oxygen levels in the blood, improving overall function. In severe cases, mechanical ventilation becomes necessary to maintain gas exchange. Evidence-based guidelines highlight its importance in life-threatening cardiogenic pulmonary edema (CPE). Non-invasive ventilation often yields better outcomes by avoiding intubation, reducing risks like ventilator-induced lung injury (VILI).
- Mechanical ventilation supports gas exchange in critical CPE cases.
- High airway pressures during ventilation can increase mortality risks.
- Non-invasive ventilation improves outcomes while minimizing complications.
Treating the Root Cause of Lung Fluid Buildup
Addressing the underlying cause is essential for long-term recovery. For example, heart failure-induced pulmonary edema requires medications to strengthen the heart. Infections demand antibiotics, while trauma-related cases may need surgical intervention. Dialysis remains a supportive measure when kidney failure contributes to fluid overload, but it cannot replace targeted treatments for specific conditions.
Lifestyle and Preventative Measures
Managing Fluid Intake and Diet

Proper dietary management and fluid intake control significantly improve outcomes for patients with pulmonary edema. A conservative fluid strategy reduces the risk of respiratory failure and shortens ICU stays. Studies show that patients adhering to dietary guidelines experience better oxygenation and reduced hospital stays.
| Study Focus | Findings |
|---|---|
| Fluid overload in critically ill patients | Correlation with increased mortality and respiratory failure. |
| Conservative fluid management | Lower in-hospital mortality and improved respiratory outcomes. |
| Randomized study by Wiedemann et al. | Reduced cumulative fluid balance and shorter ICU stays. |
Monitoring and Treating Underlying Conditions
Regular monitoring of chronic conditions like heart disease or kidney failure prevents fluid buildup. Patient education and counseling improve adherence to treatment plans, reducing the need for intensive interventions. Lifestyle changes, such as reducing salt intake and maintaining a healthy weight, further support fluid balance. These measures, combined with medical treatments like dialysis, help manage pulmonary edema effectively.
Tip: Early intervention and consistent monitoring can prevent complications and improve quality of life for patients with lung fluid issues.
Conclusion
Dialysis can help manage fluid overload, which may indirectly reduce lung fluid in certain cases. However, it does not directly remove fluid from the lungs. Pulmonary edema often requires targeted treatments, such as diuretics or oxygen therapy. Consulting healthcare providers ensures the most effective approach for managing lung fluid issues. Clinical tools like lung ultrasound, echocardiography, and bioimpedance analysis assist in evaluating fluid status and guiding treatment strategies. These methods provide valuable insights into overhydration and venous congestion, helping clinicians tailor interventions to individual needs.
