

Plasmapheresis vs. dialysis are both life-saving procedures designed to remove harmful substances from the blood, but they serve different purposes. Plasmapheresis specifically targets the plasma, removing large molecules like antibodies or toxins, and often replaces it with donor plasma or a substitute. In contrast, dialysis filters waste and excess fluids, primarily for patients with kidney failure. Global data highlights the benefits of plasmapheresis, such as a higher rate of successful treatment discontinuation (14.3% vs. 5.1%) compared to non-plasmapheresis cases. Understanding these distinctions between plasmapheresis vs. dialysis helps medical professionals determine the most effective approach for specific conditions.
Key Takeaways
- Plasmapheresis removes bad substances in plasma. It helps with autoimmune diseases like myasthenia gravis.
- Dialysis clears waste and extra fluids from blood. It is needed for people with kidney failure.
- Knowing the differences helps patients and doctors pick the best treatment for health problems.
- Plasmapheresis works fast to ease symptoms. Dialysis is a long-term fix for kidney problems.
- Talking to doctors helps people make smart choices about treatments and risks.
What Is Plasmapheresis?
Definition and Purpose of Plasmapheresis
Plasmapheresis, also known as therapeutic plasma exchange, is a medical procedure that separates plasma from the blood. This process is designed to remove harmful substances, such as antibodies, toxins, or abnormal proteins, from the plasma. It is particularly effective in treating autoimmune disorders like myasthenia gravis, Guillain-Barre syndrome, and chronic inflammatory demyelinating polyneuropathy. Additionally, it is used for managing complications of sickle cell disease and certain neuropathies.
The primary goal of plasmapheresis is to replace unhealthy plasma with healthy plasma or a substitute. This exchange helps reduce the concentration of harmful molecules, alleviating symptoms and improving the patient’s condition. For autoimmune disorders, plasmapheresis can provide symptom relief within days. However, some conditions may require weeks of therapy to show noticeable improvements. Repeated sessions are often necessary to maintain long-term benefits.
How Plasmapheresis Works?
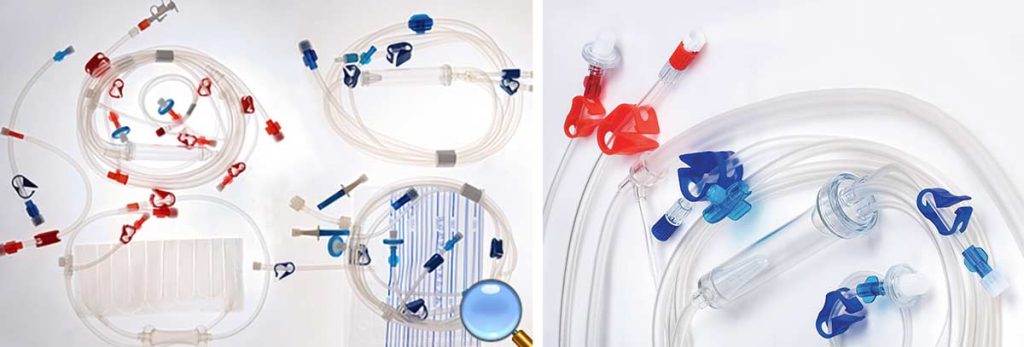
The plasma exchange procedure involves withdrawing blood from the patient and separating it into its components—red blood cells, white blood cells, platelets, and plasma. A specialized machine performs this separation. Once the plasma is removed, it is replaced with donor plasma, a plasma substitute, or a combination of both. The treated blood is then returned to the patient’s body.
This process targets large molecules in the plasma, such as autoantibodies or immune complexes, which contribute to disease progression. By removing these substances, plasmapheresis helps restore balance in the immune system. For example, in conditions like thrombotic thrombocytopenic purpura or Goodpasture syndrome, this therapy can significantly improve outcomes.
Several clinical studies validate the effectiveness of plasmapheresis. For instance, a meta-analysis by Vamvakas et al. highlights its success in treating chronic progressive multiple sclerosis. Another study by van Der Meche and Schmitz compares plasmapheresis with intravenous immune globulin for Guillain-Barre syndrome, emphasizing its therapeutic value. These findings underscore the importance of plasmapheresis in managing complex medical conditions.
What Is Dialysis?
Definition and Purpose of Dialysis
Dialysis is a medical procedure that artificially removes waste products, toxins, and excess fluids from the blood when the kidneys fail to perform these functions. It is also known as renal replacement therapy (RRT). This treatment becomes necessary when a person loses 85 to 90 percent of kidney function. Without dialysis, waste accumulation in the blood can lead to severe health complications, including organ failure.
Healthy kidneys filter approximately 120 to 150 quarts of blood daily, maintaining a balance of electrolytes and fluids. When kidney function declines, dialysis steps in to replicate this vital process. In the United States, around 14 percent of the population is affected by chronic kidney disease (CKD), highlighting the importance of this life-saving therapy. Dialysis not only helps manage kidney failure but also improves the quality of life for patients awaiting kidney transplants.
How Dialysis Works?
Dialysis operates by mimicking the natural filtration process of healthy kidneys. There are two primary types of dialysis: hemodialysis and peritoneal dialysis. Hemodialysis involves using a machine to filter the blood. A vascular access point, such as an arteriovenous fistula, connects the patient to the machine. Blood is drawn, filtered through a dialyzer to remove waste and excess fluids, and then returned to the body. This process typically occurs three times a week, with each session lasting about four hours.
Peritoneal dialysis, on the other hand, uses the lining of the abdomen (peritoneum) as a natural filter. A special fluid is introduced into the abdominal cavity through a catheter. The fluid absorbs waste and toxins before being drained and replaced. This method can be performed at home, offering greater flexibility for patients.
Innovative technologies continue to enhance dialysis efficiency and patient outcomes. For example, bioengineered human acellular vessels improve vascular access, while wearable hemodialysis machines provide mobility during treatment. Devices like multiple-frequency bio-impedance systems aid in fluid management, ensuring optimal care for dialysis patients. Additionally, vitamin E-coated membranes used in hemodialysis reduce oxidative stress, further improving patient safety.
Statistical studies emphasize the importance of stable hemodynamic conditions during dialysis. Measurements of cardiac index and blood flow rates during hemodialysis sessions reveal how precise adjustments can optimize treatment. These advancements underscore the critical role of dialysis in managing kidney failure and improving patient well-being.
Plasmapheresis vs Dialysis: Key Differences
Differences in Purpose
Plasmapheresis and dialysis serve distinct purposes in medical treatment. Plasmapheresis, also known as therapeutic plasma exchange, focuses on removing harmful substances from the plasma. This procedure targets large molecules such as autoantibodies, immune complexes, or abnormal proteins that contribute to autoimmune or blood-related disorders. By replacing unhealthy plasma with donor plasma or a substitute, therapeutic plasmapheresis helps restore balance in the immune system. It is commonly used for conditions like myasthenia gravis, Guillain-Barre syndrome, and thrombotic thrombocytopenic purpura.
Dialysis, on the other hand, addresses kidney failure by replicating the filtration function of healthy kidneys. It removes waste products, toxins, and excess fluids from the blood. This treatment is essential for patients with chronic kidney disease or acute kidney injury. Unlike plasmapheresis, dialysis does not replace plasma but instead focuses on maintaining the body’s electrolyte and fluid balance. It is often a long-term solution for individuals awaiting kidney transplants.
Differences in Processes
The processes involved in plasmapheresis and dialysis differ significantly. Plasmapheresis involves separating blood into its components—red blood cells, white blood cells, platelets, and plasma. A specialized machine extracts the plasma, which is then replaced with donor plasma or a plasma substitute. The treated blood is returned to the patient, completing the cycle. This procedure specifically targets the removal of harmful substances present in the plasma.
Dialysis operates through two primary methods: hemodialysis and peritoneal dialysis. Hemodialysis uses a machine to filter the blood externally. Blood is drawn from the patient, passed through a dialyzer to remove waste and excess fluids, and then returned to the body. Peritoneal dialysis, in contrast, uses the peritoneum (the lining of the abdomen) as a natural filter. A special fluid introduced into the abdominal cavity absorbs waste and toxins before being drained and replaced.
The duration and complexity of these procedures also vary. Plasmapheresis typically takes 1.5 to 4 hours per session, depending on the method used. For example, centrifugal therapeutic plasma exchange (cTPE) averages 110 minutes, while membrane therapeutic plasma exchange (mTPE) can take up to 240 minutes. Dialysis sessions, particularly hemodialysis, usually last about four hours and occur three times a week. Peritoneal dialysis offers more flexibility, as it can be performed at home.
| Procedure Type | Average Duration (minutes) | Effectiveness Notes |
|---|---|---|
| Centrifugal TPE (cTPE) | 110 | Shorter procedure times and fewer complications compared to membrane TPE (mTPE) |
| Membrane TPE (mTPE) | 240 | Longer procedure duration, potentially more complications |
Differences in Targeted Substances
Plasmapheresis and dialysis target different substances within the blood. Plasmapheresis focuses on removing large molecules found in the plasma. These include autoantibodies, immune complexes, and abnormal proteins that contribute to autoimmune diseases and other conditions. By extracting these harmful substances, therapeutic plasmapheresis helps alleviate symptoms and slow disease progression.
Dialysis, in contrast, targets smaller waste products and toxins that accumulate in the blood due to kidney failure. These substances include urea, creatinine, and excess electrolytes like potassium and sodium. Dialysis also removes excess fluids to prevent complications such as swelling or high blood pressure. Unlike plasmapheresis, dialysis does not address issues related to the immune system or plasma composition.
The differences in targeted substances highlight the unique roles of these procedures. Plasmapheresis is ideal for conditions involving abnormal plasma components, while dialysis is essential for managing kidney-related issues.
When Is Each Treatment Recommended?
Factors Influencing the Choice of Plasmapheresis
Plasmapheresis is recommended when conditions involve abnormal plasma components that contribute to disease progression. Autoimmune disorders, such as myasthenia gravis and Guillain-Barre syndrome, often require this procedure. It is also effective for managing blood-related conditions like thrombotic thrombocytopenic purpura. The decision to use plasmapheresis depends on the severity of the condition, the presence of specific autoantibodies, and the patient’s overall health.
Contraindications play a critical role in determining whether plasmapheresis is suitable. Patients with severe hypocalcemia, unstable cardiovascular conditions, or active infections may not tolerate the procedure well. Medical professionals assess these contraindications carefully to minimize risks. Additionally, the availability of donor plasma or substitutes influences the feasibility of this treatment. In some cases, repeated sessions are necessary to achieve optimal results.
The timing of plasmapheresis is another important factor. Early intervention often leads to better outcomes, especially in acute conditions. For example, initiating plasmapheresis promptly in cases of Goodpasture syndrome can prevent irreversible organ damage. By targeting harmful substances in the plasma, this procedure offers a targeted approach to managing complex medical conditions.
Factors Influencing the Choice of Dialysis
Dialysis becomes essential when kidney function declines to a critical level. Patients with chronic kidney disease or acute kidney injury often rely on this treatment to remove waste, toxins, and excess fluids from the blood. The choice between hemodialysis and peritoneal dialysis depends on several factors, including the patient’s lifestyle, medical history, and vascular access.
Clinical metrics play a significant role in determining the need for dialysis. Measurements such as Kt/V, Urea Reduction Ratio (URR), and biochemical markers guide treatment decisions. The table below highlights the percentage of studies that emphasize these metrics:
| Metric | Percentage of Studies (%) |
|---|---|
| Kt/V | 87 |
| Urea Reduction Ratio (URR) | 58 |
| Biochemical Measures | 95 |
| Patient-Relevant Outcomes | 2 |
Patients often express gratitude for dialysis, as it prolongs their lives. However, they also consider factors like quality of life, time spent on dialysis, and the friendliness of medical staff. These aspects influence their perception of the treatment’s adequacy. Contraindications, such as severe infections or unstable cardiovascular conditions, may limit the use of dialysis. In such cases, alternative treatments of renal disorders may be explored.
Role of Medical Professionals in Decision-Making

Medical professionals play a pivotal role in determining the most appropriate treatment for each patient. They evaluate the indications and contraindications of plasmapheresis and dialysis, considering the patient’s medical history, current condition, and treatment goals. Their expertise ensures that the chosen procedure aligns with the patient’s needs and minimizes potential risks.
Doctors often collaborate with specialists to develop a comprehensive treatment plan. For plasmapheresis, hematologists and immunologists may provide insights into the patient’s plasma composition and immune response. For dialysis, nephrologists assess kidney function and recommend the most suitable dialysis method. This multidisciplinary approach enhances the effectiveness of the treatment.
Patient education is another critical aspect of decision-making. Medical professionals explain the benefits, risks, and expected outcomes of each procedure, empowering patients to make informed choices. They also address concerns about contraindications and provide guidance on managing side effects. By fostering open communication, healthcare providers build trust and ensure that patients feel supported throughout their treatment journey.
Conclusion
Plasmapheresis and dialysis serve unique roles in medical care. Plasmapheresis focuses on removing harmful substances from plasma, making it effective for autoimmune and blood-related disorders. Dialysis, however, addresses kidney failure by filtering toxins and waste from the blood. Each procedure targets specific medical needs, ensuring tailored treatment for patients.
Understanding the differences between these treatments helps patients make informed decisions. Medical professionals guide this process, explaining the risks and benefits. By learning about the purposes and processes of plasmapheresis and dialysis, individuals can better navigate their healthcare options.
