
Dialysis plays a critical role in replacing kidney function for patients with end-stage renal disease. For some individuals, opting for dialysis twice a week may seem appealing due to fewer sessions and potential cost savings. However, this approach carries risks that require careful consideration. Studies during the COVID-19 pandemic revealed that patients on dialysis twice a week experienced increased pre-dialysis blood pressure and potassium levels, though these remained within safe limits. This highlights the importance of close monitoring and individualized treatment plans. Consulting a healthcare provider ensures that any changes to dialysis frequency, including switching to dialysis twice a week, prioritize safety and health outcomes.
Key Takeaways
- Doing dialysis only twice a week can cause harmful toxins to build up. This can lead to problems like uremia or high potassium.
- Less dialysis may make the body hold too much fluid. This can cause high blood pressure and stress on the heart.
- Dialysis patients need a treatment plan made just for them. They should talk to their doctor before changing how often they do dialysis.
- Some people feel better with fewer dialysis sessions, but it doesn’t work for everyone.
- Patients doing dialysis twice a week must watch their health closely. This helps avoid serious health problems.
The Role of Kidney Dialysis in the Body
Removing Toxins and Waste Products
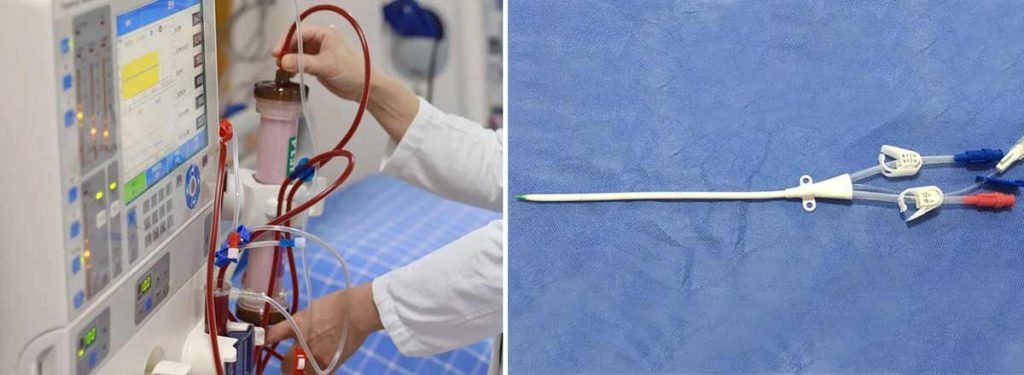
Kidney dialysis plays a vital role in removing toxins and waste products from the bloodstream. When kidneys fail, they can no longer filter harmful substances like urea and creatinine effectively. These toxins accumulate in the body, leading to a condition called uremia, which can cause nausea, fatigue, and confusion. Hemodialysis helps prevent these symptoms by mimicking the kidney’s filtration process. During each session, a machine removes blood from the body, filters it through a dialyzer, and returns it, free of toxins. This process is essential for maintaining a stable internal environment and preventing long-term complications.
Managing Fluid Levels and Preventing Overload
Dialysis also helps regulate fluid levels in the body. Patients with kidney failure often struggle to maintain fluid balance, as their kidneys cannot remove excess water. Fluid overload can result in swelling, difficulty breathing, and even heart strain. Hemodialysis removes this excess fluid, reducing the risk of these complications. Studies show that optimal fluid management is crucial for avoiding poor health outcomes. Advanced tools like lung ultrasounds and bioimpedance analysis are increasingly used to assess fluid status more accurately. Additionally, limiting sodium and fluid intake between sessions helps patients maintain appropriate fluid levels.
Supporting Overall Health and Reducing Complications
Regular dialysis sessions contribute to overall health by reducing the risk of complications associated with kidney failure. For instance, thrice-weekly hemodialysis has been linked to lower interdialytic weight gain and improved survival rates compared to twice-weekly sessions. While twice-weekly dialysis may reduce costs, it often results in higher hospitalization rates and increased strain on the body. Maintaining a consistent dialysis schedule ensures better toxin removal, fluid balance, and overall well-being, highlighting the importance of personalized treatment plans tailored to each patient’s needs.
Risks of Dialysis Twice a Week
Toxin Buildup and Its Consequences
Reducing the frequency of hemodialysis to twice a week can lead to the dangerous accumulation of toxins in the body. These toxins, such as potassium and urea, are typically removed during dialysis sessions. When toxin accumulation occurs, patients may experience symptoms of uremia, including nausea, fatigue, and confusion. Studies have shown that reduced dialysis frequency often results in higher pre-dialysis potassium levels. While most patients maintain safe levels, potassium levels above 6.0 mmol/L significantly increase the risk of mortality. This highlights the importance of regular dialysis to prevent toxin buildup and its associated health risks.
Fluid Retention and Related Health Issues

Twice-weekly dialysis may also lead to fluid retention, which can cause severe complications. Dialysis patients undergoing fewer sessions often experience greater interdialytic weight gains due to excess fluid accumulation. This can result in pulmonary edema, high blood pressure, and increased strain on the heart. Clinical data indicates that patients on twice-weekly schedules tend to have higher ultrafiltration volumes per session. Large fluid shifts during dialysis can contribute to left ventricular hypertrophy and congestive heart failure. Managing fluid intake and maintaining an appropriate dialysis schedule are critical for reducing these risks.
| Dialysis Frequency | UF Volume (liters/session) | Hospitalizations for Fluid Overload |
|---|---|---|
| Twice Weekly | 1.4 (1.0–2.0) | None |
| Thrice Weekly | 1.5 (1.0–2.0) | N/A |
Increased Risk of Hospitalization and Emergencies
Patients on a twice-weekly dialysis schedule face a higher likelihood of hospitalization and emergency events. Approximately 40% of these patients require hospitalization, compared to 37.7% of those on a thrice-weekly schedule. Although the difference is not statistically significant, the reduced frequency of dialysis increases the risk of emergencies due to toxin buildup and fluid retention. Personalized treatment plans and close monitoring by healthcare providers can help mitigate these risks and improve patient outcomes.
Potential Benefits of Twice-Weekly Hemodialysis
Preservation of Residual Kidney Function
Twice-weekly hemodialysis may help preserve residual kidney function (RKF) in select patients. Studies suggest that reducing the frequency of dialysis can minimize the strain on remaining kidney function, allowing it to perform essential tasks like removing toxins and maintaining fluid balance. Patients with higher RKF often experience better health-related quality of life (HRQOL) due to improved phosphorus excretion, reduced inflammation, and more effective fluid and salt removal.
- Research highlights the following benefits of preserving RKF:
- Reduced pro-inflammatory mediators, leading to better overall health.
- Improved survival rates among patients with higher RKF.
- Enhanced ability to manage fluid and electrolyte levels naturally.
During the COVID-19 pandemic, some patients safely transitioned to dialysis twice a week for at least one month. Close monitoring ensured that while certain parameters increased, they remained within safe limits. This demonstrates that reducing dialysis frequency can be a viable option for carefully selected individuals.
Fewer Intra-Dialytic Complications
Twice-weekly hemodialysis may result in fewer complications during sessions. Patients undergoing less frequent dialysis often experience reduced episodes of low blood pressure, cramping, and fatigue during treatment. This is because the body undergoes fewer rapid fluid and toxin shifts, which can strain the cardiovascular system.
A study conducted in Alexandria Governorate found that patients with preserved RKF on a twice-weekly schedule had comparable hospitalization rates to those on thrice-weekly dialysis. This suggests that reducing session frequency can lower the risk of complications without compromising safety for certain individuals. However, careful patient selection and monitoring remain critical to achieving these outcomes.
| Study | Findings |
|---|---|
| Alexandria Governorate | Twice-weekly HD showed similar hospitalization rates to thrice-weekly HD for patients with RKF. |
| Hanson et al. | Twice-weekly HD patients had a 24% lower adjusted mortality and better quality of life. |
Improved Quality of Life for Select Patients
For some patients, twice-weekly hemodialysis offers a better quality of life. Fewer sessions mean less time spent traveling to dialysis centers and undergoing treatment, which can reduce stress and improve mental well-being. Additionally, the financial burden of treatment decreases, benefiting both patients and healthcare systems.
Studies show that dialysis patients on a twice-weekly schedule experienced similar hospitalization rates (40%) compared to those on thrice-weekly dialysis (37.7%). This indicates that reducing frequency does not necessarily lead to worse outcomes for select individuals. Moreover, the reduction in governmental and out-of-pocket costs makes this approach more accessible for patients with financial constraints.
Note: While twice-weekly hemodialysis can improve quality of life for some, it is not suitable for everyone. Patients must work closely with their healthcare providers to determine the best treatment plan based on their individual needs and health status.
Patient Experiences and Medical Insights
Variability in Individual Needs
Factors That May Allow Reduced Frequency
Patients undergoing twice-weekly hemodialysis often exhibit diverse responses due to individual health conditions. Factors such as residual kidney function, urine output exceeding 0.5 liters per day, and stable electrolyte levels may allow some individuals to safely reduce their dialysis frequency. However, variability in patient outcomes remains significant. For instance:
- Median systolic blood pressure increased from 145 mmHg to 153 mmHg after three weeks of twice-weekly dialysis.
- Pre-dialysis potassium levels rose slightly from 4.5 mmol/L to 4.7 mmol/L.
- The number of patients with dangerously high potassium levels above 6.0 mmol/L increased over time.
These findings highlight the importance of monitoring patients closely to ensure safety when reducing dialysis sessions to twice a week.
Insights from Nephrologists
Importance of Personalized Treatment Plans
Nephrologists emphasize the need for personalized treatment plans when considering twice-weekly hemodialysis. Clinical studies reveal that this regimen may not provide optimal control of fluid volume, electrolytes, and urea levels. Patients must meet specific criteria, such as maintaining adequate urine output and stable health indicators, to qualify for reduced frequency.
| Evidence Type | Description |
|---|---|
| Clinical Outcome | Twice-weekly HD often results in poorer control of key health parameters. |
| Prescription Criteria | Patients must meet strict health criteria for reduced frequency. |
| Economic Considerations | Lower costs make twice-weekly dialysis appealing in resource-limited settings. |
| Limitations | Studies often face challenges like unequal sample sizes and varying care quality. |
Nephrologists also stress the importance of balancing cost savings with patient safety. While twice-weekly hemodialysis reduces expenses, it requires careful evaluation to avoid compromising health outcomes.
Stories from Patients
Challenges and Successes with Twice-Weekly Dialysis

Dialysis patient experiences with twice-weekly dialysis vary widely. Some individuals report improved quality of life due to fewer sessions and reduced financial strain. Others face challenges such as increased fluid retention and higher toxin levels.
| Aspect | Twice-Weekly Dialysis | Thrice-Weekly Dialysis |
|---|---|---|
| Economic Burden | Reduced costs | Higher costs |
| Patient Acceptance | Well-accepted | Not specified |
| Survival Outcomes | No effect | Not specified |
| Duration of Treatment | Can continue > 2 years | Not specified |
For many, the reduced frequency offers a sense of normalcy and freedom. However, close monitoring and individualized care remain essential to address potential complications and ensure long-term success.
Conclusion
Dialysis twice a week may work for patients with significant residual kidney function. However, it poses serious risks for others. Hemodialysis removes toxins and excess fluid, which helps maintain balance in the body. Reducing the frequency of hemodialysis can lead to dangerous complications, including toxin buildup and fluid retention. These issues may strain the heart and other organs. Dialysis patients should always consult their nephrologist to create a treatment plan tailored to their specific needs. Personalized care ensures safety and improves long-term outcomes.
FAQ
What Is Dialysis, And Why Is It Necessary?
Dialysis replaces kidney function by removing toxins, waste, and excess fluid from the blood. It is essential for patients with kidney failure because their kidneys cannot perform these tasks effectively, leading to dangerous health complications.
Can Patients Safely Reduce Dialysis To Twice A Week?
Some patients with residual kidney function may tolerate twice-weekly dialysis. However, this approach requires close monitoring to ensure toxin levels and fluid balance remain stable. Consulting a nephrologist is crucial before making changes.
What Are The Risks Of Skipping Dialysis Sessions?
Skipping dialysis sessions can lead to toxin buildup, fluid retention, and strain on the heart. These complications increase the risk of emergencies, including pulmonary edema and uremia, which can be life-threatening.
How Does Dialysis Frequency Affect Quality Of Life?
Fewer dialysis sessions may improve quality of life for some patients by reducing travel and treatment time. However, this benefit depends on individual health conditions and requires careful evaluation to avoid compromising safety.
Are There Financial Benefits To Twice-Weekly Dialysis?
Twice-weekly dialysis can lower treatment costs for patients and healthcare systems. However, the potential savings must be balanced against the risks of reduced toxin removal and fluid management, which may lead to higher hospitalization rates.
