

Peritoneal dialysis relies on specialized catheters to facilitate effective treatment. Choosing the right catheter significantly impacts patient outcomes. For instance, studies show that early peritonitis episodes occurred in only 2.6% of patients using peritoneoscopic catheters compared to 12.5% in those with surgical catheters. Survival rates also improved, with 51.3% of peritoneoscopic catheter users surviving at 36 months versus 36% for surgical users. Understanding peritoneal dialysis catheter types helps patients and healthcare providers select options that minimize complications and enhance long-term success.
Key Takeaways
- Picking the right dialysis catheter helps patients feel better and stay healthier.
- The Tenckhoff catheter works well, but it can cause infections. Patients must keep it clean.
- Swan-Neck catheters stay in place better and last longer.
- Presternal catheters are good for people with special needs, like obesity. They lower infection risks by exiting on the chest.
- Talk to your doctor to choose the best catheter for your health and daily life.
Types of Peritoneal Dialysis Catheters
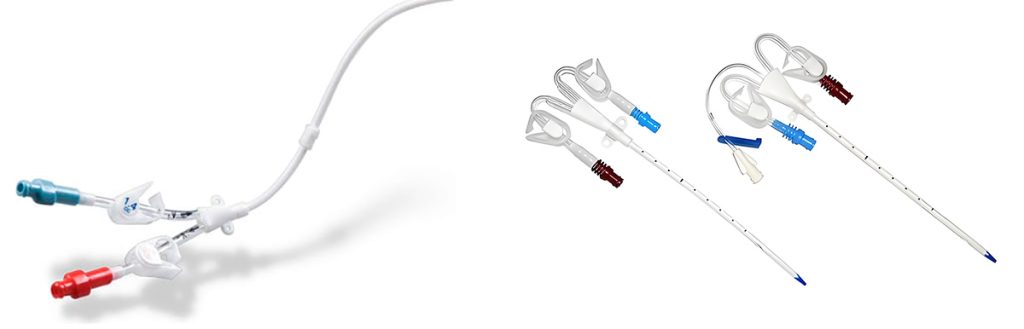
Tenckhoff Catheter
The Tenckhoff catheter is one of the most commonly used peritoneal dialysis catheter types. It features a straight or coiled design, with a silicone tube that allows for effective fluid exchange during peritoneal dialysis. This catheter is typically inserted surgically or laparoscopically, ensuring proper placement in the peritoneal cavity.
Clinical studies highlight its reliability. For instance, randomized controlled trials show that delaying peritoneal dialysis initiation by two weeks after Tenckhoff catheter insertion reduces complications. Observational studies also support this approach, emphasizing lower infection rates and improved outcomes. Guidelines from organizations like CARI recommend this delay to enhance patient safety.
The Tenckhoff catheter’s coiled design minimizes the risk of migration, ensuring stable positioning. However, it may require careful monitoring to prevent complications such as peritonitis or exit-site infections.
Swan-Neck Catheter
The Swan-Neck catheter is designed to reduce complications associated with traditional straight catheters. Its curved shape prevents catheter migration and minimizes the risk of cuff extrusion. This catheter is often preferred for patients requiring long-term peritoneal dialysis.
Research supports its benefits. A study comparing Swan-Neck and straight catheters found a lower incidence of pericatheter leakage and cuff extrusion in the Swan-Neck group. Additionally, modifying the catheter to include a presternal exit site has shown increased access survival rates, with up to 95% success at two years. The design also reduces tip migration, enhancing overall functionality.
Despite its advantages, the Swan-Neck catheter may require more precise placement techniques. Proper training for healthcare providers ensures optimal outcomes for dialysis patients.
Presternal Catheter
The Presternal catheter offers a unique solution for patients with specific needs, such as those with ostomies or obesity. Its exit site is located on the chest, away from the abdominal area, reducing the risk of infection. This design makes it a suitable option for patients who may face challenges with traditional catheter placements.
Evidence suggests that presternal catheters significantly lower infection risks. By positioning the exit site away from potential contamination sources, these catheters provide a safer alternative for certain patient groups. However, they may not be suitable for all individuals, as the placement process can be more complex.
Patients considering a presternal catheter should consult their healthcare provider to determine if this option aligns with their medical history and lifestyle.
Pigtail Catheter
The pigtail catheter is a specialized option for peritoneal dialysis. Its name comes from the coiled, pig-tail-like shape at the catheter’s tip. This design helps anchor the catheter in place, reducing the risk of migration within the peritoneal cavity. The pigtail catheter is often chosen for its ability to maintain a stable position during treatment.
One of the key features of the pigtail catheter is its flexibility. The coiled tip minimizes irritation to the peritoneal lining, which can enhance patient comfort. Additionally, the design promotes efficient fluid exchange, making it a reliable choice for various types of dialysis. Healthcare providers often recommend this catheter for patients who require long-term peritoneal dialysis.
The pigtail catheter offers several advantages. Its unique shape reduces the likelihood of complications such as leakage or blockage. Patients using this catheter often report fewer issues with tip migration compared to other designs. Furthermore, the insertion process is relatively straightforward, which can simplify the procedure for both dialysis patients and medical teams.
However, the pigtail catheter is not without its challenges. The coiled tip may occasionally make removal more difficult, especially if the catheter has been in place for an extended period. Proper training for healthcare providers is essential to ensure safe and effective use. Patients should also follow their care team’s instructions to minimize the risk of infection or other complications.
Features, Pros, and Cons of Peritoneal Dialysis Catheter Types
Tenckhoff Catheter: Features, Advantages, and Disadvantages
The Tenckhoff catheter is a widely used option among peritoneal dialysis catheter types. Its design includes a straight or coiled silicone tube, which facilitates effective fluid exchange. This catheter is typically inserted surgically or laparoscopically to ensure proper placement in the peritoneal cavity.
Advantages:
- The coiled design minimizes the risk of migration, ensuring stable positioning.
- Studies show a low catheter dysfunction rate of 0%, with 93.15% of catheters retained in patients over time.
- It is suitable for most patients, including those with a history of abdominal surgery.
Disadvantages:
- The risk of peritonitis remains a concern, with a reported rate of 16.44%.
- Patients may experience exit-site infections if proper hygiene is not maintained.
| Feature | Detail |
|---|---|
| Catheter dysfunction rate | 0% |
| Peritonitis rate | 16.44% |
| Retained catheters | 93.15% |
Swan-Neck Catheter: Features, Advantages, and Disadvantages
The Swan-Neck catheter features a curved design that reduces complications like migration and cuff extrusion. This catheter is often chosen for long-term peritoneal dialysis.
Advantages:
- The low entry-site design prevents catheter migration.
- Three cuffs provide additional protection against peritonitis.
- Studies indicate fewer obstruction episodes compared to straight Tenckhoff catheters.
Disadvantages:
- Placement requires precision, which may necessitate specialized training for healthcare providers.
- The curved design may not suit all dialysis patients, depending on their anatomy.
A Cochrane meta-analysis found minimal differences in risks of peritonitis, exit-site infection, or catheter failure between straight and coiled catheters. However, the Swan-Neck catheter’s innovative design offers added stability and protection.
Presternal Catheter: Features, Advantages, and Disadvantages
The Presternal catheter is designed for patients with unique needs, such as those with ostomies or obesity. Its exit site is located on the chest, away from the abdominal area, reducing infection risks.
Advantages:
- The chest exit site minimizes contamination from abdominal sources.
- It is a safer option for dialysis patients with obesity or previous abdominal surgeries.
Disadvantages:
- Placement is more complex and may require advanced surgical techniques.
- Not all patients are suitable candidates for this catheter type.
| Pros of Peritoneal Dialysis | Cons of Peritoneal Dialysis |
|---|---|
| Can be done at home after training, allowing for flexible scheduling. | Risk of infection, such as peritonitis, if the catheter site is contaminated. |
| Equipment is portable and can be automated for convenience. | Potential for decreased effectiveness due to thickening or scarring of the abdominal membrane. |
The Presternal catheter provides a unique solution for specific patient groups, but careful consideration of individual needs is essential before selection.
Pigtail Catheter: Features, Advantages, and Disadvantages
The pigtail catheter stands out due to its unique coiled tip, which helps anchor it securely within the peritoneal cavity. This design minimizes the risk of migration and enhances stability during peritoneal dialysis. Its flexibility also reduces irritation to the peritoneal lining, improving patient comfort.
Advantages:
- The coiled tip ensures stable positioning, reducing the likelihood of mechanical complications.
- Patients report fewer issues with catheter malfunction compared to other designs.
- The insertion process is straightforward, making it a preferred choice for many healthcare providers.
Disadvantages:
- The coiled tip can complicate removal, especially after prolonged use.
- Proper training for healthcare providers is essential to ensure safe handling and minimize risks.
Note: The pigtail catheter’s design promotes efficient fluid exchange, making it a reliable option for long-term dialysis. However, patients must follow strict hygiene protocols to prevent infections.
| Evidence Type | Details |
|---|---|
| Complication Rate | 30% experienced mechanical complications with Tenckhoff catheters compared to pigtail catheters. |
| Preference Rate | 80% of colleagues preferred pigtail catheters due to ease of insertion and lower malfunction rates. |
The table above highlights the pigtail catheter’s advantages over the Tenckhoff catheter. Its lower complication rate and ease of insertion make it a popular choice among healthcare professionals. Despite its benefits, dialysis patients should consult their care team to determine if this catheter aligns with their medical needs and lifestyle.
Factors to Consider When Choosing a Peritoneal Dialysis Catheter
Patient Lifestyle and Daily Activities
A patient’s lifestyle plays a critical role in selecting the appropriate peritoneal dialysis catheter. Individuals who engage in active daily routines or physical activities may benefit from catheters designed for stability, such as the Swan-Neck or pigtail catheter. These designs minimize the risk of migration, ensuring the catheter remains securely in place during movement.
For patients who prefer home-based treatments like continuous ambulatory peritoneal dialysis or continuous cyclic peritoneal dialysis, catheter placement and exit site location are essential considerations. A presternal catheter, for example, may suit individuals who require a chest exit site to reduce the risk of contamination during daily activities.
Patients should also consider the potential impact of their catheter choice on clothing and comfort. Catheters with coiled designs, such as the Tenckhoff or pigtail catheter, often provide greater flexibility and comfort, making them suitable for long-term use.
Medical History and Specific Health Conditions
A patient’s medical history and existing health conditions significantly influence catheter selection. Factors such as previous abdominal surgeries, obesity, or the presence of ostomies may limit the suitability of certain catheter types. For instance, a presternal catheter is often recommended for patients with abdominal scarring or obesity, as its chest exit site avoids the abdominal area.
Clinical parameters, including blood pressure, disease severity, and laboratory results, also guide catheter choice. Patients with diabetes or prolonged dialysis duration may face higher risks of complications, such as peritonitis or catheter dysfunction. A systematic review highlights that older age, diabetes, and low serum albumin levels increase the likelihood of peritonitis-related treatment failure. These factors emphasize the need for careful evaluation before catheter placement.
| Predictor | Description |
|---|---|
| Socio-demographic characteristics | Includes age, sex, mobility, and dialysis modality (e.g., intermittent peritoneal dialysis) |
| Clinical presentation | Blood pressure, symptoms, and disease severity during peritonitis episodes |
| Laboratory tests | Dialysate leukocyte count and causative organism |
Doctor Recommendations and Clinical Considerations

Healthcare providers play a vital role in guiding patients toward the most suitable catheter. Doctors base their recommendations on clinical guidelines, patient anatomy, and the risk of possible complications of peritoneal dialysis. For example, consensus guidelines emphasize evidence-based practices to reduce catheter-associated infections.
Studies reveal that catheter duration is a primary risk factor for complications, such as catheter-associated urinary tract infections (CAUTI). Targeted interventions, including proper catheter care and regular monitoring, can mitigate these risks. Additionally, healthcare providers consider the patient’s dialysis modality, such as continuous ambulatory peritoneal dialysis or continuous cyclic peritoneal dialysis, when recommending a catheter type.
Dialysis patients should actively discuss their concerns and preferences with their care team. This collaborative approach ensures that the chosen catheter aligns with the patient’s medical needs and lifestyle, ultimately improving treatment outcomes.
Conclusion
Understanding the peritoneal dialysis catheters types is essential for improving treatment outcomes. Personalized decision-making plays a pivotal role in selecting the right catheter. For instance, a study of 29 patients with obesity using extended peritoneal dialysis catheters showed no intraoperative complications and high survival rates over two years.
| Evidence Type | Description |
|---|---|
| Study Cohort | 29 patients with obesity receiving 31 intraperitoneally extended PD catheters |
| Median BMI | 35.5 kg/m² (range 26.4–46.9) |
| Complications | No intraoperative complications; 1 seroma and 1 dialysate leakage postoperatively |
| Survival Rates | High 1-year and 2-year catheter survival rates |
Consulting healthcare providers ensures better outcomes. Research highlights that increased nurse staffing significantly reduces mortality and hospitalizations, underscoring the value of professional guidance. Dialysis patients should work closely with their care teams to make informed choices tailored to their needs.
